Can a Hole in a Heart Happen Again
Overview
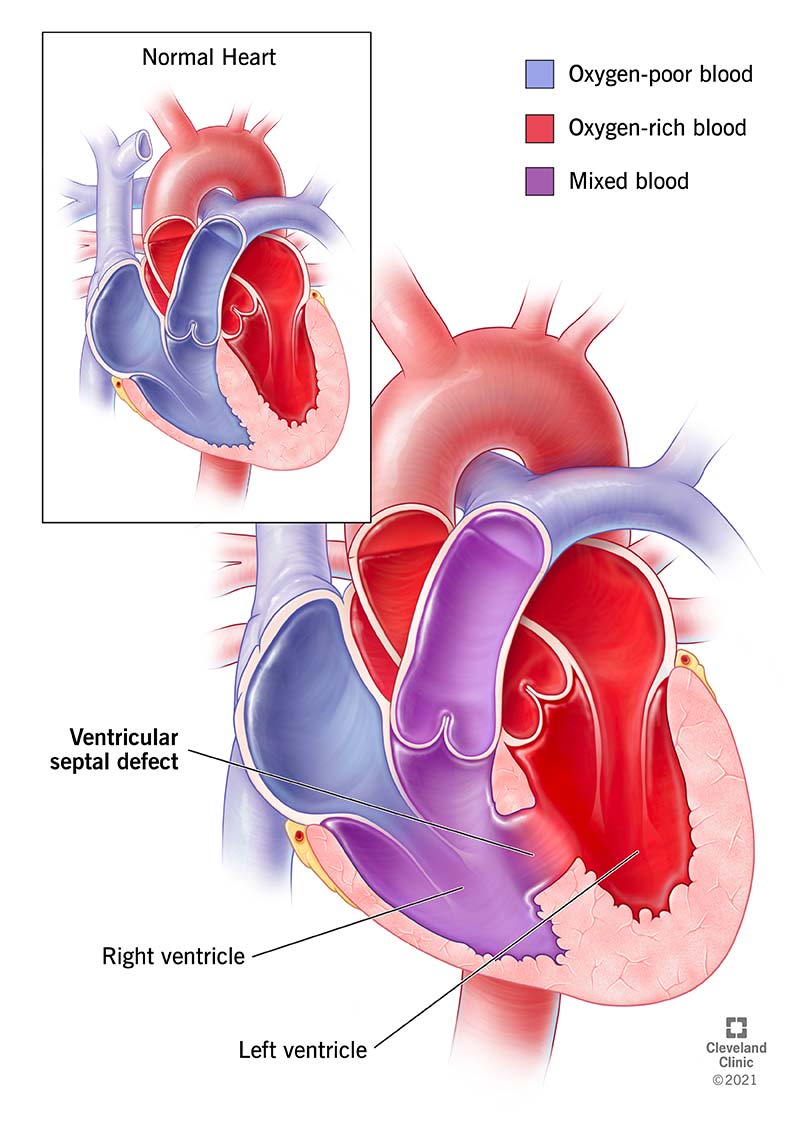
What is a ventricular septal defect?
A ventricular septal defect is a condition where you lot're built-in with a hole in the wall between the two lower chambers of your heart. Often shortened to VSD, this status is the nearly common built (meaning you have information technology when you're built-in) centre defect and frequently happens aslope other types of heart problems or defects. A small VSD is normally minor and has few or no symptoms. Even so, a larger pigsty may need to be repaired to avoid permanent impairment and complications.
What happens inside my heart if I accept a ventricular septal defect?
Your eye has iv chambers. To pump claret efficiently, the chambers much seal shut. A VSD is a leak that disrupts that efficient pumping ability.
Under normal circumstances, the right ventricle pumps oxygen-poor blood that but arrived from your torso out of your heart and into your lungs and so the blood can pick upward oxygen. The blood so returns to the eye, and its last stop in the eye is the left ventricle, which pumps oxygen-rich blood out to your entire body.
A VSD is a potential problem because information technology can act equally a shunt (a connection) betwixt the centre's ii lower chambers, the left ventricle and the right ventricle. Considering the pressure level in the left ventricle is higher than the pressure level in the right ventricle, oxygen-rich claret mixes with oxygen-poor blood in the right ventricle and and then goes to the lungs. That leads to extra blood in the lungs which can cause serious issues.
Who does information technology affect?
Almost all VSDs are present at birth. A VSD diagnosis most probable happen during childhood, though adults tin besides receive this diagnosis. Even so, this only happens in 10% or less of cases. VSD is as well slightly more probable to happen in premature babies and babies with certain genetic conditions.
In very rare cases, a heart assail can tear a hole betwixt the ventricles and create a VSD. While this type of VSD — sometimes called ventricular septal rupture (VSR) — is technically a side effect, information technology is still a dangerous problem that needs to be repaired.
How common is this status?
VSD happens in about ane-third of 1% of all newborns. Yet, a VSD diagnosis in adults is much less likely because the defect closes on its own during babyhood in 90% of cases.
VSDs that are a side effect of a heart attack are extremely rare, especially because of modernistic heart assail treatment methods. Today, it happens in less than 1% of all heart attacks.
What are the different types of VSD?
There are four main types of VSD, which differ in their location and the construction of the hole (or holes). The types of VSD are:
- Membranous: This is the most common blazon of VSD and makes up well-nigh 80% of cases. These VSDs happen in the upper department of the wall betwixt the ventricles.
- Muscular: These account for virtually 20% of VSDs in infants, and there is often more one hole that'southward role of the defect.
- Inlet: This is a hole that happens just below the tricuspid valve in the correct ventricle and the mitral valve in the left ventricle. That means when claret enters the ventricles, information technology must pass a VSD that connects the two chambers.
- Outlet (conoventricular): This kind of VSD creates a hole only before the pulmonary valve in the right ventricle and but before the aortic valve in the left ventricle, connecting the ii chambers. That means blood has to go past the VSD on its way through both valves.
How does this condition affect my trunk?
VSD doesn't crusade symptoms in nearly cases because the hole isn't large enough to crusade bug. Yet, in cases where the hole is large enough (or if there are multiple holes), it can cause problems with claret leaking between the two chambers instead of circulating through the heart in the correct order.
That leaking makes your heart's pumping efforts less efficient, though if the leak is smaller, it may not be enough to cause any symptoms or bug. However, your eye needs to pump harder to compensate for the reduced blood flow when the leak is larger. When your heart works harder like that long-term, it can cause symptoms and bug in the centre and lungs that may become astringent.
VSD size and effects
VSDs range in size from small to large, with the size playing a role in what effects — if whatsoever — the VSD will crusade.
- Pocket-sized (3 mm in diameter or less): About VSDs fall in this category and don't cause symptoms. Nigh nine out of x of this type will close on their ain by the time a kid is 6 years onetime. Surgery for these is rare.
- Moderate (3-v mm in diameter): These VSDs don't ordinarily crusade symptoms. If they aren't causing symptoms or problems elsewhere in the heart and lungs, delaying surgery is usually advised considering some also close on their own.
- Large (6-10 mm in diameter): These VSDs oftentimes require surgery (the timing of the surgery tin vary slightly). Repair of a large VSD earlier age 2 tin can prevent damage to the eye and lungs. Without repair before historic period ii, the damage becomes permanent and gets worse over time.
When a moderate or large VSD is not treated in time, Eisenmenger syndrome tin develop. This is a condition where long-term impairment to blood vessels in the lungs forces oxygen-poor blood from the right ventricle through a large VSD and into the left ventricle. That ways some of the blood pumped to the torso doesn't contain plenty oxygen. That causes an overall oxygen shortage throughout the body. This condition is typically severe and can take major consequences on a person's life and the activities in which they tin can participate.
The left ventricle has greater pumping strength than the right, which means it can strength blood into the right ventricle. The right ventricle tin't push the extra blood back, so the extra blood instead gets pumped into the lungs. That puts likewise much pressure on and amercement the lung'southward blood vessels. Over time, the damage in the lung'southward blood vessels starts to force the leak in the center to reverse direction, forcing oxygen-poor blood from the right ventricle into the left.
Once the management of the leak reverses, the impairment is permanent and repairing the hole volition crusade right-sided eye failure. Surgical repair of a moderate or large VSD before age 2 is vital to prevent permanent harm and developing Eisenmenger syndrome.
Symptoms and Causes
What are the symptoms?
In infants, moderate to large VSD causes symptoms that expect like heart failure. These include:
- Shortness of breath, including fast breathing or struggling to exhale.
- Sweating or fatigue during feeding.
- Failure to thrive (wearisome weight proceeds).
- Frequent respiratory infections.
VSD in older children and adults tin cause the following:
- Feeling tired or out of breath easily when exercising.
- Slightly higher risk of heart inflammation caused by infections.
- Later Eisenmenger syndrome develops, very pale skin or a bluish tinge to pare and lips (a condition called cyanosis) may happen.
What causes the condition?
VSD that'south present at birth doesn't currently have any known causes. Still, it does sometimes happen along with other heart defects, center weather condition or genetic disorders. Taking certain anti-seizure medications (sodium valproate and phenytoin) or drinking alcohol during pregnancy may besides increase the risk of your child developing a VSD. Even so, it will have more inquiry to confirm if these are definite causes.
The only known cause of VSD is when it happens as a rare side effect of a heart attack.
Diagnosis and Tests
How is it diagnosed?
A physician tin diagnose a VSD — especially when they're moderate- or big-sized — based on a combination of symptoms, a physical exam and imaging tests. A small-scale VSD may go undetected when the hole is too small to cause signs or symptoms.
A concrete examination is ane of the about common means for a doctor to discover a VSD. That'due south because a VSD — when it's large enough —causes a sound called a centre murmur that your doctor can hear when listening to your centre with a stethoscope. Information technology'south even possible to estimate the size of the defect from the sound of a murmur.
What tests volition be done to diagnose this status?
Other tests that help diagnose VSD include the following imaging tests:
- Echocardiogram: This exam sends ultra-high-frequency sound waves through your body from a device held confronting the skin of your chest. Those sound waves create a picture of the inside and outside of the heart. Depending on the size of the VSD and its exact location, information technology's probable to be visible on an echocardiogram. This test is as well painless and only takes minutes to complete.
- Electrocardiogram (ECG or EKG): This test uses multiple sensors attached to the skin of your chest to detect the electric activity of your eye. That activity appears every bit a moving ridge on a printout or digital display for a healthcare provider to review and interpret. Over fourth dimension, your heart structure can modify because of a VSD. When the structure changes, the electrical pattern too changes. However, this test volition often be normal if the VSD isn't large enough or if the middle hasn't started to change shape.
- Chest or middle Ten-ray: When a VSD is large enough, it will cause the structure of your middle to change. That change is visible on certain types of chest or heart Ten-rays. In some cases, it also involves injecting a substance into the blood that is hands visible on 10-rays, which allows healthcare providers to encounter any unusual claret apportionment that indicates a VSD or other problem.
- Computed tomography (CT) scan: This test uses a calculator to process X-ray images into a three-dimensional motion picture of the within of the heart. Like with a chest or heart X-ray, an injectable substance that's highly visible on a CT scan may help.
- Cardiac catheterization: This procedure uses a catheter device to look at the middle from the inside. A specialist inserts the device into a major blood vessel, commonly one near your upper thigh, and then passes it upwardly to your centre. One time within your eye, information technology can help pinpoint the size and location of any problems like a VSD. The virtually probable reason to employ this examination is when a healthcare provider suspects blood vessel harm in the lungs.
Management and Treatment
How is it treated, and is there a cure?
The majority of VSDs are too modest to cause any kind of problem, and they volition likely close on their own by historic period 6. In those cases, a healthcare provider is likely to recommend against surgery, propose monitoring for symptoms and meet if the defect closes independently. When VSDs are moderate-sized or larger, your md will likely recommend repairing the VSD by closing the hole.
The two principal ways to repair a VSD are:
- Surgery: The most reliable way to shut a VSD is to patch it surgically. To do this, a cardiac (heart) surgeon will operate and patch or close the hole. Depending on the size and location of the hole, it may be as simple as stitching the hole close. In other cases, it might involve a patch made of a synthetic cloth or a graft of your own tissue.
- Transcatheter procedures: Like cardiac catheterization, these procedures use a transcatheter (catheter-based) approach to access the heart via a major artery. One time the catheter device reaches the defect, it tin can identify a specialized device called an occluder and plug the hole. These devices are typically made of a mesh framework covered in a synthetic material.
In either of the above cases, your center tissue volition abound over and around the patch or occlude device. Ultimately, the patch or device should become part of the heart wall between the ventricles.
In cases where an infant or child is underweight or isn't growing at the expected rate, their healthcare provider may recommend special measures to assist them get enough nutrition. This might include a special nutrition or even a feeding tube.
What medications/treatments are used?
Medication tin care for symptoms of a VSD before surgery or if the VSD is likely to shut on its own over time. Mutual medications for VSD are often the aforementioned as those that treat center failure. They include:
- Diuretics: These medications increment the amount of fluid your kidneys remove from your body. This is helpful when fluid is building up around your heart, a common effect of heart failure. These medications may brand you urinate (pee) more oftentimes.
- Center failure medications: These medications help control the strength and timing of your heartbeats. An case is digoxin, a mutual medication in the treatment of eye failure that is likewise helpful for VSD.
What are the possible complications or side effects of the treatments?
In general, your healthcare provider is the all-time person to explain the potential risks, complications and side effects that are possible with a VSD or related procedures and treatments. This is especially true for any recommended medications.
Mutual side effects or complications from surgery or transcatheter procedures for a VSD include:
- Haemorrhage.
- Infections, particularly centre infections within the first six months after surgery.
- Disruption of nearby heart valves, causing them to leak.
- Center rhythm problems (arrhythmias and centre blocks), which might lead to implantation of a pacemaker or indefinite treatment with medication.
- Follow-upward surgery to close a recurring hole.
How shortly after treatment will I feel better, and how long does it take to recover from this handling?
Recovery from repair of a VSD depends on the method used. Transcatheter procedures take shorter recovery times, with recovery times measured in days or weeks. Surgeries take longer recovery times, measured in weeks or months. Symptoms of a VSD usually decrease or disappear after surgery or transcatheter repairs.
Prevention
How can I forestall this condition or reduce my risk?
Considering there aren't whatsoever known causes for VSD, prevention isn't commonly possible. However, you can subtract the risk past avoiding booze employ and certain anti-seizure medications during pregnancy.
Outlook / Prognosis
What can I expect if I have this condition?
Most adults with a VSD don't know about it because information technology isn't large enough to crusade any problems. However, the larger the VSD, the more likely it will affect how you lot alive your life, especially if it isn't repaired.
How long does a VSD final?
Approximately xc% of VSDs volition close on their own past the fourth dimension a person turns 6 years old. Most of the remaining 10% of VSDs will close by age 20. However, a VSD is unlikely to close on its own after that.
An adult with a VSD will take it for the rest of their life unless they undergo a procedure to repair it.
What'southward the outlook for this condition?
Most people with a VSD have the same life expectancy as someone who doesn't accept one. This is especially truthful if the defect closes on its own.
In cases of a moderate or big VSD, repair of the hole is unremarkably enough to prevent Eisenmenger syndrome and related issues. In rare cases, a follow-upward surgery becomes necessary to close new leaks effectually the repair. Unfortunately, virtually people with a moderate or large VSD — even one that's repaired —are more probable to take a lower life expectancy, specially if the VSD was not repaired early.
For people who have a VSD that isn't repaired, nearly 87% of them volition exist alive 25 years subsequently their diagnosis. The size of the VSD has a major effect on the odds of survival, withal.
- Small: Small VSDs are unlikely to accept a major affect on your life. Overall, 96% of people with an unrepaired small defect live more than 25 years after diagnosis.
- Moderate: Survival rates for people with unrepaired moderate VSDs are a little fleck lower, with about 86% of them surviving at least 25 years after diagnosis.
- Large: Survival rates for people with a large unrepaired VSD are much lower. Simply about 61% of these individuals are still alive 25 years later their diagnosis.
People who develop Eisenmenger syndrome from a moderate or large VSD tend to have the worst survival outlook. Only about 42% of these individuals will exist alive at least 25 years after their diagnosis with a VSD. Notwithstanding, advancements in modern medicine are improving the outlook for individuals with this condition and some live to be in their 70s.
Living With
How can I take care of myself and manage my symptoms?
Overall, yous should ask your healthcare provider for guidance on managing your symptoms and taking intendance of yourself. Their advice volition exist all-time suited to you because they tin can see the overall picture show of your health and medical situation and tailor the guidance they give you accordingly.
If you lot take symptoms because of a VSD, your healthcare provider will likely advise you to rest and avert too much physical activity or any activeness that puts too much strain on your center. This is especially true if you have Eisenmenger syndrome related to an untreated VSD. You should too be sure to accept medications exactly as instructed and only change or stop taking medications if you have talked to your healthcare provider and they have confirmed information technology's safe to practise so.
When should I see my healthcare provider?
When yous don't know virtually a VSD
If you accept an infant that doesn't have a VSD that yous know of, yous should talk to their healthcare provider if y'all notice any of the post-obit symptoms:
- Slower than expected growth or weight gain.
- Sweating or getting tired while feeding.
- If they are very fussy or show signs of trouble animate.
- If they have frequent respiratory infections.
If you are an adult and aren't enlightened that y'all have a VSD, y'all should talk to your healthcare provider if you notice that y'all get tired or short of jiff hands when you're physically active, or if you are ofttimes stake or observe a blue tint to your fingertips or lips.
When y'all know well-nigh a VSD
If your child has a VSD, their healthcare provider can advise y'all on potential signs and symptoms of VSD-related bug. In full general, look for the same symptoms of VSD that are described above. You should besides talk to their healthcare provider if yous detect any sudden or unusual changes in their existing symptoms.
If you lot have a VSD, you should also talk to your healthcare provider if you lot have any sudden changes in your symptoms. You should also talk to a healthcare provider about your status before you have any surgery or dental work to make sure they know about your condition.
When should I go to the ER?
Your healthcare provider or the provider caring for your child can explicate when y'all should become emergency medical care for symptoms that are or might exist related to a VSD. In general, you should become to the emergency room if you or your kid have trouble animate or any signs of cyanosis (pale or bluish skin, lips or fingernails).
A annotation from Cleveland Dispensary
If you or your kid have a ventricular septal defect, it's normal to experience concerned, anxious or even scared. If you're dealing with these kinds of feelings, it'due south a good idea to talk to your healthcare provider or the provider caring for your child. They can help you improve sympathize the condition and what to expect. More chiefly, they can help y'all find ways to treat this condition, forestall complications and minimize how it affects the life of y'all or your child.
Source: https://my.clevelandclinic.org/health/diseases/17615-ventricular-septal-defects-vsd
0 Response to "Can a Hole in a Heart Happen Again"
Post a Comment